$ 0.000 -15.66%
Verasity (VRA) Rank 3095
| Mkt.Cap | $ 2.41 M | Volume 24H | 19.48 BVRA |
| Market share | 0% | Total Supply | 0.00000000VRA |
| Proof type | PoW | Open | $ 0.000029 |
| Low | $ 0.000024 | High | $ 0.000029 |
How to Use Veracity vs. voracity Correctly – Grammarist
Have you ever wondered how nurses or other health care providers make difficult decisions regarding their patients' lives? Each health care provider abides by a code of ethics that regulates his or her behavior. Ethics relates to moral principles and actions. Some believe most medical practitioners in the future will have to be or greatly benefit from being bilingual.
However, as some of the examples in this study session have shown, you will be faced with dilemmas that are difficult to resolve in harmony with the concepts of respecting autonomy and informed consent, and reconciling the demands of beneficence and nonmaleficence. In Study Session 8 there will be further examples of ethical dilemmas for you to think about and learn from.
What are the 8 ethical principles?
Bioethicists often refer to the four basic principles of health care ethics when evaluating the merits and difficulties of medical procedures. Ideally, for a medical practice to be considered "ethical", it must respect all four of these principles: autonomy, justice, beneficence, and non-maleficence.
For the 1803 textbook, see Medical Ethics (book). For the journal, see Journal of Medical Ethics.
The term refers to every individual’s right of self-determination, independence and freedom to make their own choices. In the context of healthcare, the concept of autonomy is most concerned with the ethical obligation of the practitioner to respect their clients’ right to make decisions about their own health. Autonomy must be respected even if you, as the healthcare provider, do not agree with the client’s decision. For example, in Case Study 7.1, Chaltu may feel that Almaz’s parents should know what has happened to their daughter, but you must respect Almaz’s right to maintain confidentiality about her condition. Some of these are difficult words, but in this study session you will be able to consider each of them in turn, using examples that will be familiar to you.

Aboriginal elder; a layman; a laywoman; a lawyer and, in the case of a hospital-based ethics committee, a nurse. On the other hand, autonomy and beneficence/non-maleficence may also overlap. For example, a breach of patients' autonomy may cause decreased confidence for medical services in the population and subsequently less willingness to seek help, which in turn may cause inability to perform beneficence. The term beneficence refers to actions that promote the well being of others.

Examples of Antonyms

The Declaration provides special protection of human rights for incompetent persons. The human rights era started with the formation of the United Nations in 1945, which was charged with the promotion of human rights. The Universal Declaration of Human Rights (1948) was the first major document to define human rights. Medical doctors have an ethical duty to protect the human rights and human dignity of the patient so the advent of a document that defines human rights has had its effect on medical ethics.[32] Most codes of medical ethics now require respect for the human rights of the patient.
What is the difference between honesty and truthfulness?
Honesty and truthfulness are not the same thing. Being honest means not telling lies. Being truthful means actively making known all the full truth of a matter. But if they unknowingly say something that isn't true, they are being honest.
However, many other societies prioritize beneficence over autonomy. James Childress and Tom Beauchamp in Principle of Biomedical Ethics (1978) identify beneficence as one of the core values of healthcare ethics. Some scholars, such as Edmund Pellegrino, argue that beneficence is the only fundamental principle of medical ethics. They argue that healing should be the sole purpose of medicine, and that endeavors like cosmetic surgery and euthanasia are severely unethical and against the Hippocratic Oath. Veracity is defined as being honest and telling the truth and is related to the principle of autonomy.
British Dictionary definitions for truthfulness
Confidentiality is an important issue in primary care ethics, where physicians care for many patients from the same family and community, and where third parties often request information from the considerable medical database typically gathered in primary health care. All nurses abide by a set of ethical principles that guide their actions and behaviors.


Everyone should have access to the same things that might improve their health. As a Health Extension Practitioner, you will be able to carry out distributive and social justice by enabling the inclusion and empowerment of all people living within your area to exercise their rights (Figure 7.6). You can understand the concept of justice from the examples in Case Study 7.2.
- For this patient, it would be practicing beneficence for the nurse to advocate for the patient and arrange for cancer treatment to be stopped.
- Interested in linking to or reprinting our content?
- This will enable you to identify some of the most important ethical issues and then find out how to work to resolve them.
- What is the difference between distributive justice and social justice?
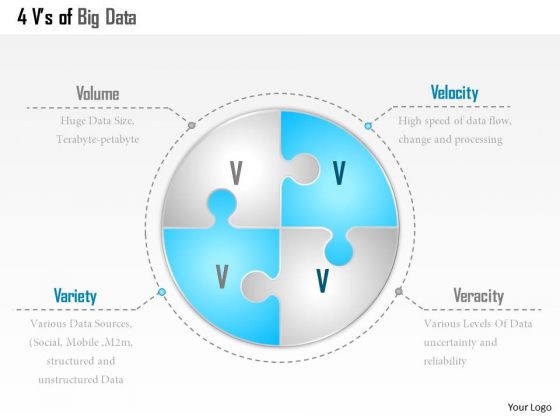
Data veracity is the degree to which data is accurate, precise and trusted. The reality of problem spaces, data sets and operational environments is that data is often uncertain, imprecise and difficult to trust.
What is the formal definition of justice?
Formal justice is the impartial, consistent and strict application of established rules or laws; material justice concerns the justice or injustice of the content of rules or laws.
Individuals' capacity for informed decision-making may come into question during resolution of conflicts between autonomy and beneficence. The role of surrogate medical decision makers is an extension of the principle of autonomy. Respect for autonomy – the patient has the right to refuse or choose their treatment.
Origin of veracity
What is DHMO found in?
For those who have become dependent, DHMO withdrawal means certain death. Dihydrogen monoxide: is also known as hydroxyl acid, and is the major component of acid rain. contributes to the "greenhouse effect."
Informed consent means that each person who has any sort of procedure done to them in a healthcare context should give their approval for that procedure to be done to them. In order to be fully informed, it is the duty of the healthcare worker to tell the person exactly what the procedure will involve as well as the things that might happen if the procedure is not carried out.

Beneficence should not be confused with the closely related ethical principle of nonmaleficence, which states that one should not do harm to patients. This principle acts as an obligation for nurses to protect their patients from harm by removing and preventing bad situations and promoting good ones.
In this section you will be able to learn about two important ethical concepts which may be new to you, but which are relevant for your practice. These are called beneficence and nomaleficence.

This will help you to see how ethical principles are present in almost every aspect of your health work and daily life. Alene Burke RN, MSN is a nationally recognized nursing educator. She began her work career as an elementary school teacher in New York City and later attended Queensborough Community College for her associate degree in nursing.
6 ugly healthcare truths as told by nurses

How do you use vernacular in a sentence?
Sentence Examples He loved using the vernacular, although it never sounded quite right coming from him.
For example, a patient wishes to withdraw cancer treatment because he feels his quality of life is more important than living longer. For this patient, it would be practicing beneficence for the nurse to advocate for the patient and arrange for cancer treatment to be stopped. Even if the nurse wants the patient's treatment to continue, she must put the patient's idea of a good life ahead of her own. If you are entering the nursing field, it is important to understand the ethical principles involved. Check out what beneficence is and the ways in which nurses use the principle in relation to patient care.
Is truthfulness an adjective?
adjective. telling the truth, especially habitually: a truthful person. conforming to truth: a truthful statement. corresponding with reality: a truthful portrait.
Around the world, there are different organizations that campaign to change legislation about the issue of physician-assisted death, or PAD. Examples of such organizations are the Hemlock Society of the United States and the Dignity in Dying campaign in the United Kingdom. These groups believe that doctors should be given the right to end a patient's life only if the patient is conscious enough to decide for themselves, is knowledgeable about the possibility of alternative care, and has willingly asked to end their life or requested access to the means to do so. The principles of autonomy and beneficence/non-maleficence may also be expanded to include effects on the relatives of patients or even the medical practitioners, the overall population and economic issues when making medical decisions. The United Nations Educational, Scientific and Cultural Organization (UNESCO) also promotes the protection of human rights and human dignity.